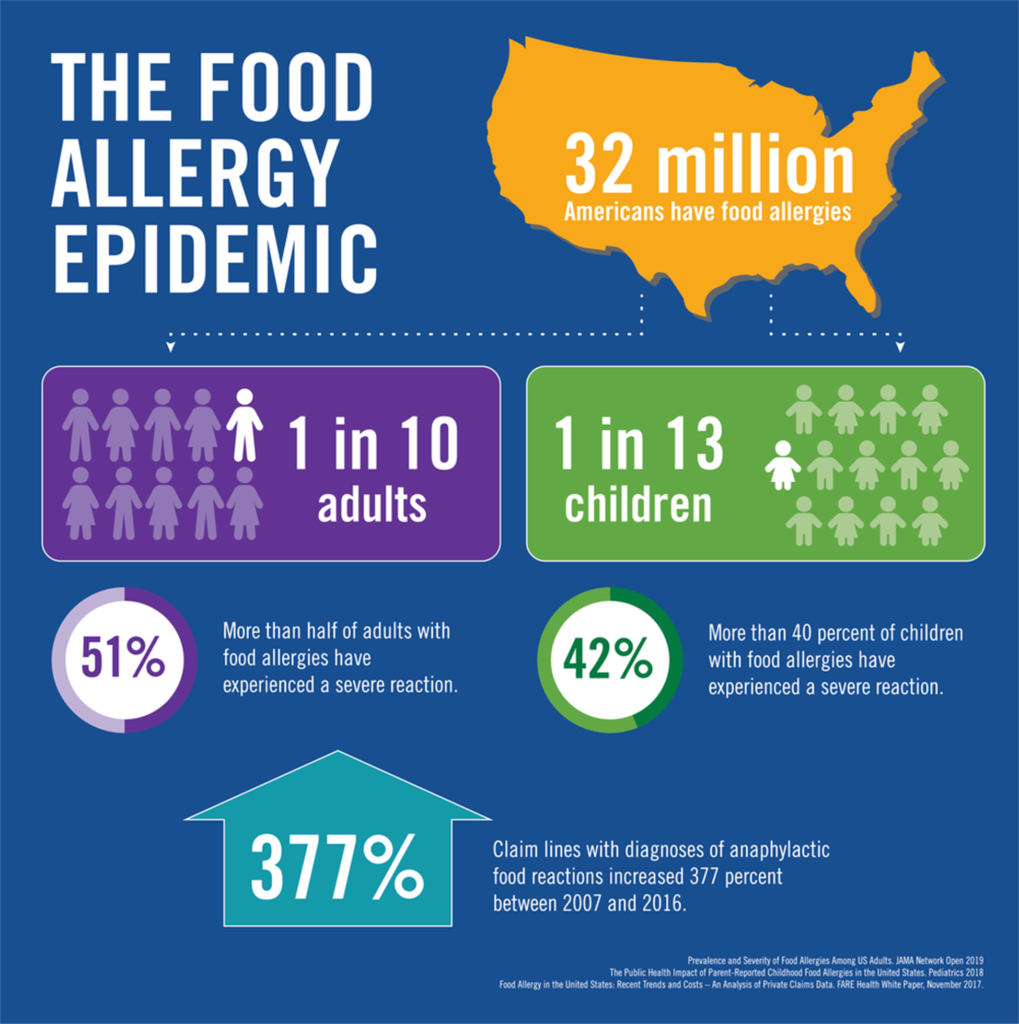
Over 32 million Americans are living with potentially life-threatening food allergies, a 377 percent increase from 2007-2016. One in 13 kids has a food allergy. The rise in food allergies is seen more in highly industrialized countries. What is the cause? While scientists believe this is multifactorial, some research supports the Hygiene Hypothesis – that our homes have become cleaner with fewer children, and higher standards of cleanliness have left children’s immune systems weaker with less practice in fighting invaders. Without practice, the immune system simply overacts. Another development is in the Dual Allergy Exposure Hypothesis, which suggests that those with eczema and scratchy skin may experience food allergens via the skin, not orally, which sensitizes the individual to mount a greater response to it. Avoiding eating possible allergens as a child and excluding them from a child’s diet may lead to a greater chance of developing allergic intolerances. A diverse range of foods should be introduced at an early age. There have also been links made from Vitamin D deficiency, and too much Vitamin D, to an increased rate of food allergy.
Family history plays a part in whether or not someone develops a food allergy, and those having eczema, asthma or hay fever, other kinds of allergic reactions, at greater risk.
Our body’s immune system is designed to protect us from foreign invaders such as viruses or bacteria. Allergic responses are when our immune system overreacts by producing allergy antibodies followed by a chemical release of histamines.
The most common food allergies are to peanuts, eggs, milk, tree nuts, soy, wheat, fish, and shellfish.
At their worst, food allergies trigger anaphylactic shock, when airways begin to swell, cutting off oxygen supply to the brain, low blood pressure, and loss of couscousness. Those with anaphylaxis often appear dizzy or disoriented because of a quick drop in blood pressure. This form of shock can lead to a coma or even death. At their mildest, food allergies may cause minor skin irritations, hives, or abdominal pain.
While there are no treatments, advances in food allergen immunotherapies are in the works. These therapies expose a patient to very small, increasing doses of the allergen, allowing the body to become slowly desensitized to the allergen until the point of toleration. Biologics are also being used alone or in combination with immunotherapies, which can block steps in the allergy pathways to limit or prevent allergic reactions. Various clinical trials are also underway. While there is no cure, some children do outgrow food allergies.
Those that suspect they have food allergies—different from food intolerances—should address it with their primary care physician. Often times, an exam, family history, symptom review, skin test (a skin prick test during which small doses of allergens are placed on the skin to see response), a blood test to measure IgE, an allergy related antibody, and exploration of an elimination diet can yield an accurate diagnosis.