Dr. Marin Gillis
Professor & Senior Executive Dean for Faculty Affairs & Learning Innovation
Interim Chair, Department of Justice & Health Humanities
Roseman College of Medicine
Often in America, health is thought of as the absence of disease or infirmity. However, for decades the World Health Organization, among others, has advocated for a more holistic understanding of what it means to be healthy, and seeks to change how we think about what health is. In the preamble to their constitution, WHO defines health as a complete state of physical, mental, and social well-being. If this is what health is, then the goals of therapeutics should not only be curative and rehabilitative, but also preventive and palliative, in the sense of managing the symptoms of chronic and life-limiting illness.
What many think of as the prime determinants of health (for example, genes, cells and biology) account for approximately 20% of health risks and outcomes. The remaining 80% is determined by:
- Access to quality healthcare
- A person’s behavior
- Social, economic, and environmental factors
Health, good or bad, is the result of actions and interactions throughout each day. The majority of these aren’t happening in what are commonly thought of as healthcare environments, but rather in the places where people live, work, and play. These factors are collectively known as the Social Determinants of Health (SDoH). Someone’s ZIP code is more of a determining factor of their health quality and lifespan than their genetic code.
The consequence of this misplaced emphasis on the biological determinants of health is evident in our health outcomes as a country. Compared to the world’s highest income nations, the U.S. has:
- Among the highest number of hospitalizations from preventable causes
- The highest rate of avoidable deaths, including suicides
- The highest chronic disease burden
- An obesity rate that is two times higher than peer nation averages
- An extremely high rate of healthcare spending – Americans spend twice as much of their income on healthcare as do citizens of our peer nations (Tikkanen 2020)
Americans spend significantly more and are less healthy largely due to a lack of understanding and emphasis on what will actually make America healthier. Hospitals largely address sickness and injury. If healthier people and better health outcomes are the goal, it is imperative to start by understanding the genesis of health as a complex of interactions between a person, their household, the communities in which they live, work and play, and policies that shape them.
The following chart shows the social and economic factors that drive health outcomes, where health outcomes are understood as mortality and morbidity, life expectancy, healthcare expenditures, and health status.
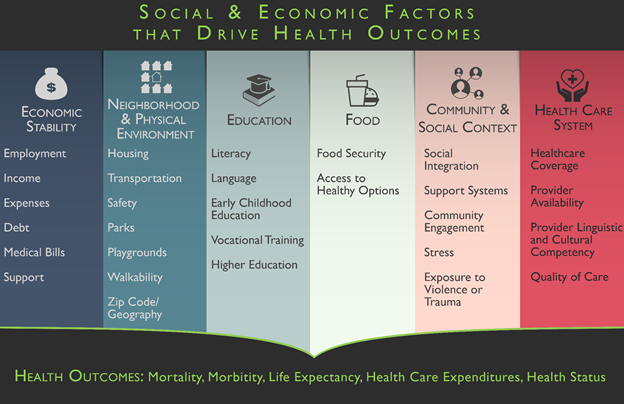
Adapted from “Health Disparities are a Symptom of Broader Social and Economic Inequities” by S. Artiga, 2020, Kaiser Family Foundation, ‘Figure 2’ (https://www.kff.org/policy-watch/health-disparities-symptom-broader-social-economic-inequities/#).
The social determinants of health are foundational concepts in Roseman University’s program development. The university is committed to transforming medical education and the health of our communities by addressing Nevada’s critical shortage of physicians through development of a revolutionary medical school. Together with his team, Dr. Pedro “Joe” Greer Jr., Presidential Medal of Freedom winner and recipient of the MacArthur Fellows Genius Grant, envisions a medical curriculum that delivers at the street level, in neighborhoods, and most importantly, in individual households. Our pioneering approach – called household centered care – gives medical students early experience in the most essential of all settings: the home.
Roseman’s College of Medicine will produce the physicians of the future, developing clinically excellent and community-based physicians. Graduates will understand the complexities of communities and how the social determinants of health impact both individual and population health. Communities will be partners in teaching and learning, giving a voice to perhaps the greatest and wisest teacher: our patients.
Medical students will join students from Roseman’s nursing, pharmacy and dental programs to address Nevada’s health inequities and lack of access to care through the GENESIS program. Launched in spring 2022, GENESIS is an educational, research, community development and healthcare delivery system. It re-conceptualizes health-aligned sectors like healthcare, public health and social services as one coordinated health ecosystem focused on the home. This patient-centered model helps students and providers track patients’ social determinants of health and connect them with direct and immediate access to care.
References
Graham, G. N. (2016). Why your ZIP code matters more than your genetic code: promoting healthy
outcomes from mother to child. Breastfeeding Medicine, 11(8), 396–397.
Tikkanen R, Abrams MK. U.S. Health Care from a Global Perspective, 2019: Higher Spending, Worse Outcomes? The Commonwealth Fund Issue Brief Jan 30, 2020.
World Health Organization (WHO). (1946). Constitution of the World Health Organization.
World Health Organization (WHO). (2020). WHO Conceptual Framework for Action on the Social Determinants of Health.