Americans refer to the “Quarantine 15”, pointing to the weight gain many experienced during the lock-down starting in March 2020 as a result of COVID-19. Add to that adjusting to our new normal as well as stress, and many continue to grapple with their weight. As we age, we experience hormonal changes, muscle loss, a more sedentary lifestyle, and a slower metabolism, all of which contribute to weight gain. Sarcopenia, a process that accelerates as we age, results in the break down of our muscles which is then often replaced with fat, which requires less energy to operate than muscle. A reduction in calorie consumption would combat this, but many of us continue our existing eating habits, which then leads to weight gain. Exercise, especially weight bearing exercise and weight training, can stimulate new muscle growth. Together with an increase in protein, we can conserve muscle and bone mass. Our hormones also fluctuate and decline as we age. Both estrogen and testosterone help regulate muscle mass and fat distribution. As we age, we also become more sedentary, sitting all day for our jobs, or commuting, and with added stress, there is less time to move. Our metabolisms slow as well and need special attention to keep them revved. If you have concerns about this issue, talk to your RMG healthcare provider.
Some quick tips include:
- Prioritize sleep – aim for 8 hours a night.
- Move – add weight bearing exercise like walking, running, or biking 2-3 times per week.
- Consider HIIT workouts, which move your heart rate in and out of different zones and help burn fat.
- Consider yoga, meditation, prayer, or other mindfulness practices to help combat stress.
- Add an additional serving of protein to your diet, and limit alcohol, sweets, and processed foods. Fill up on fruits, vegetables, and high-fiber foods.
- Be aware of your hormone levels and discuss therapies with your provider.
- Keep a journal. Journals help us more accurately report our behaviors and allow us to see meaningful trends. Writing is also therapeutic!



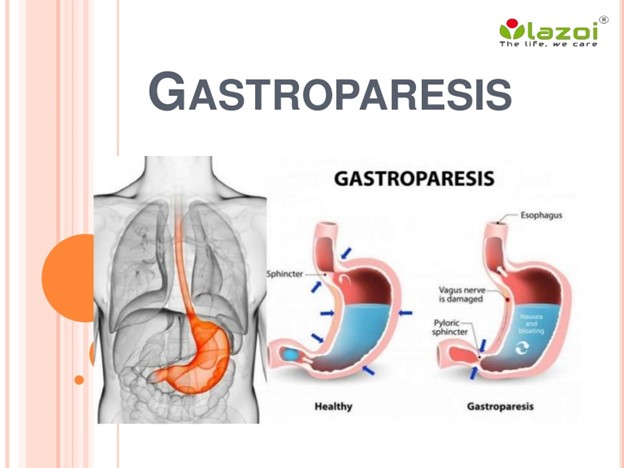












 Dr. Farbman is a gentle, affable, kind person with a natural gift for teaching and explanation. With his patients, he is patient and informative, delivering complex information in an approachable way. Active among the multiple support groups around the Valley, Dr. Farbman is truly a beacon of hope and telegraphs his optimism to his patients.
Dr. Farbman is a gentle, affable, kind person with a natural gift for teaching and explanation. With his patients, he is patient and informative, delivering complex information in an approachable way. Active among the multiple support groups around the Valley, Dr. Farbman is truly a beacon of hope and telegraphs his optimism to his patients.